SLN Mapping
Sentinel Lymph Node Biopsy
Why perform a Sentinel Lymph Node Biopsy (SLNB)?
Treating cancer involves curing disease while balancing patient comfort and pain management. Traditional cancer treatments often resulted in pain and suffering, particularly in cases such as breast or head and neck cancer.
To reduce pain and suffering, clinicians developed the Sentinel Lymph Node Biopsy (SLNB). When a cancer spreads, it typically spreads through the lymphatic system, via what are known as “Lymph Nodes.” The SLNB identifies and surgically removes the lymph nodes cancer is most likely to spread. If the nodes are determined to contain cancer, the patient’s cancer has spread and they will receive more aggressive treatment.
The SLNB is a common procedure and is used everywhere in the body. It is the standard of care for breast cancer and melanoma and is emerging in gynecologic, head and neck, prostate, and many more cancers.
What is the SLNB?
The SLNB procedure involves:
- Pre-surgical imaging to plan the surgery, which is especially important in complex anatomy such as the head and neck.
- Intra-surgical mapping to locate sentinel lymph nodes during surgery.
The “gold standard” SLNB procedure uses 99-Tc nuclear medicine.
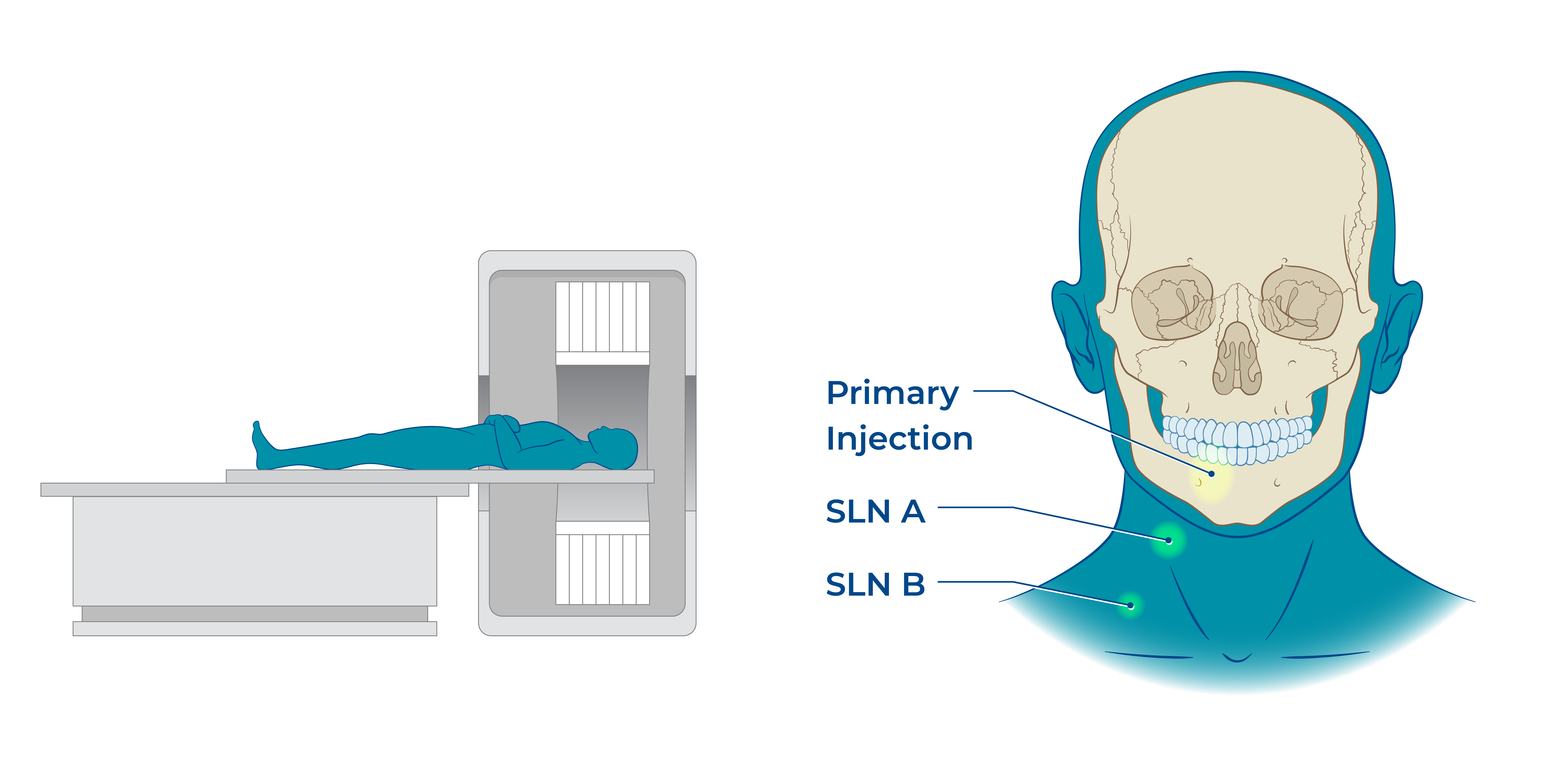
Tracer imaging is used to identify the Sentinel Lymph Nodes (SLN) using a medical imaging machine (i.e., SPECT or gamma camera).
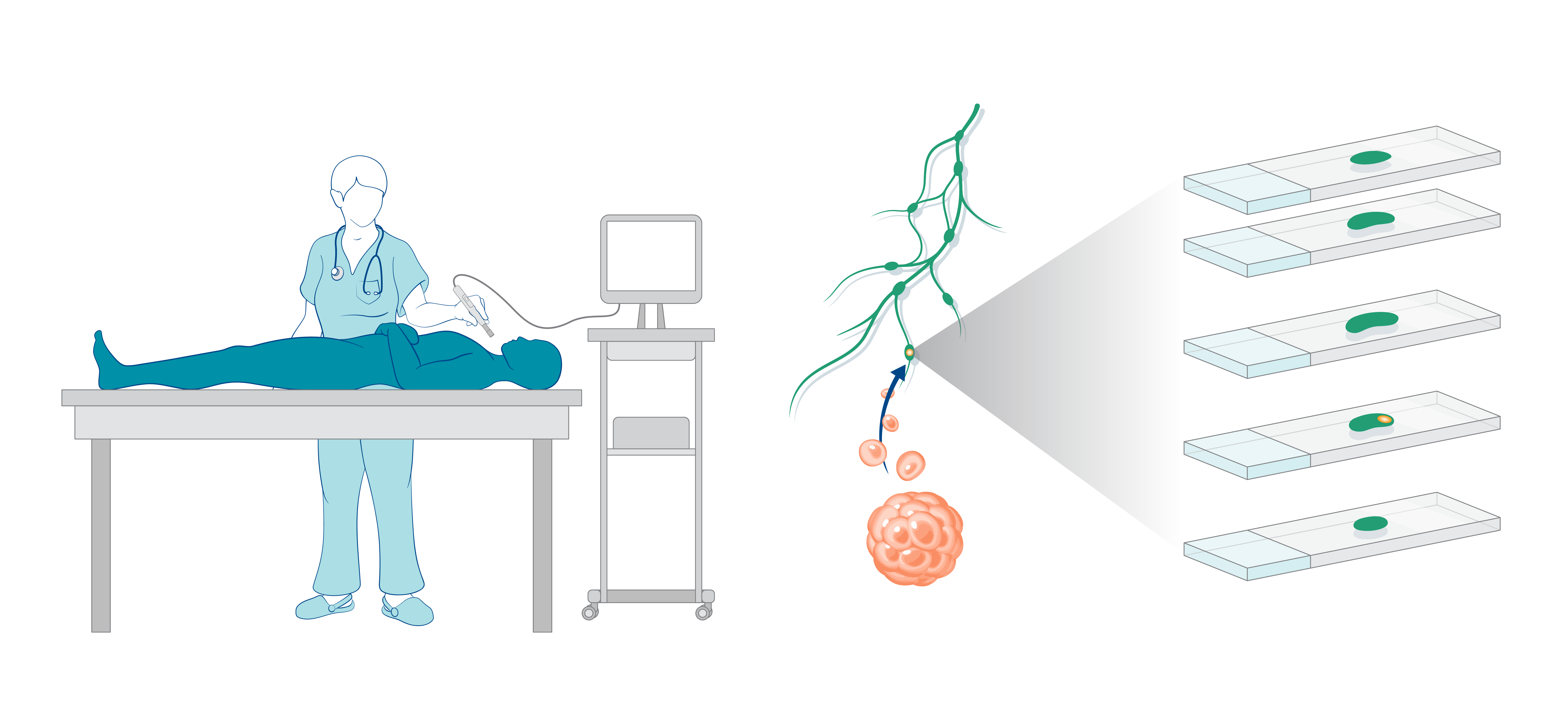
Intraoperative guidance is used to locate the node during surgery, which is then examined by the histologist on slides.
The Problems with the Current SLNB Workflow
The nuclear SLNB workflow shows efficacy, but using a nuclear tracer burdens the healthcare system with significant costs and can limit accessibility.
| Workflow step | The problem with the current SLNB workflow using 99Tc + SPECT + Gamma Wand | How MPI solves problems in the SLNB workflow | Impact |
|---|---|---|---|
| When and where the injection can occur | Imaging and surgery must be performed within 24 hours by trained personnel.Patient is admitted for 4-6 hours to isolate the public from radiation. | The tracer can be injected days in advance, including at the surgical pre-op.No special training is needed for tracer injection. | MPI requires less trips to the hospital and fewer appointments with care providers, which saves money and improves efficiency. |
| Workflow timing | All exams and surgery are within 15 minutes to 24 hours of tracer injection, or one must repeat the study. | Injection is within 20 minutes or up to 7 days (low dose) or 30 days (higher dose) before MPI imaging. | Flexibility in scheduling saves costs and adds efficiency. |
| Delayed SLNB | Does not support | Supports imaging and surgery of up to 30 days after injection, depending on tracer dosage. | A new procedure, can save upwards of 80% of SLN procedures in patients undergoing SLNB for DCIS. |
| Visual confirmation | Must be co-administered with blue dye or ICG if visual confirmation is desired. | Changes SLN color to brown, giving visual confirmation in addition to magnetic confirmation. | Reduces the number of drugs and risks associated with injectable drugs. |
MPI Solves Problems in the SLNB Workflow
Without sacrificing efficacy, our MPI technology enables a safe, non-radioactive, and widely deployable SLNB workflow without the added costs associated with nuclear medicine.
